Welcome to the PWP Corner’s section on Cognitive Restructuring.
The PWP Corner is designed for therapists. If you are not a therapist try looking at my self help section instead.
This section has two parts:
2) Information on how to guide a patient through Cognitive Restructuring.
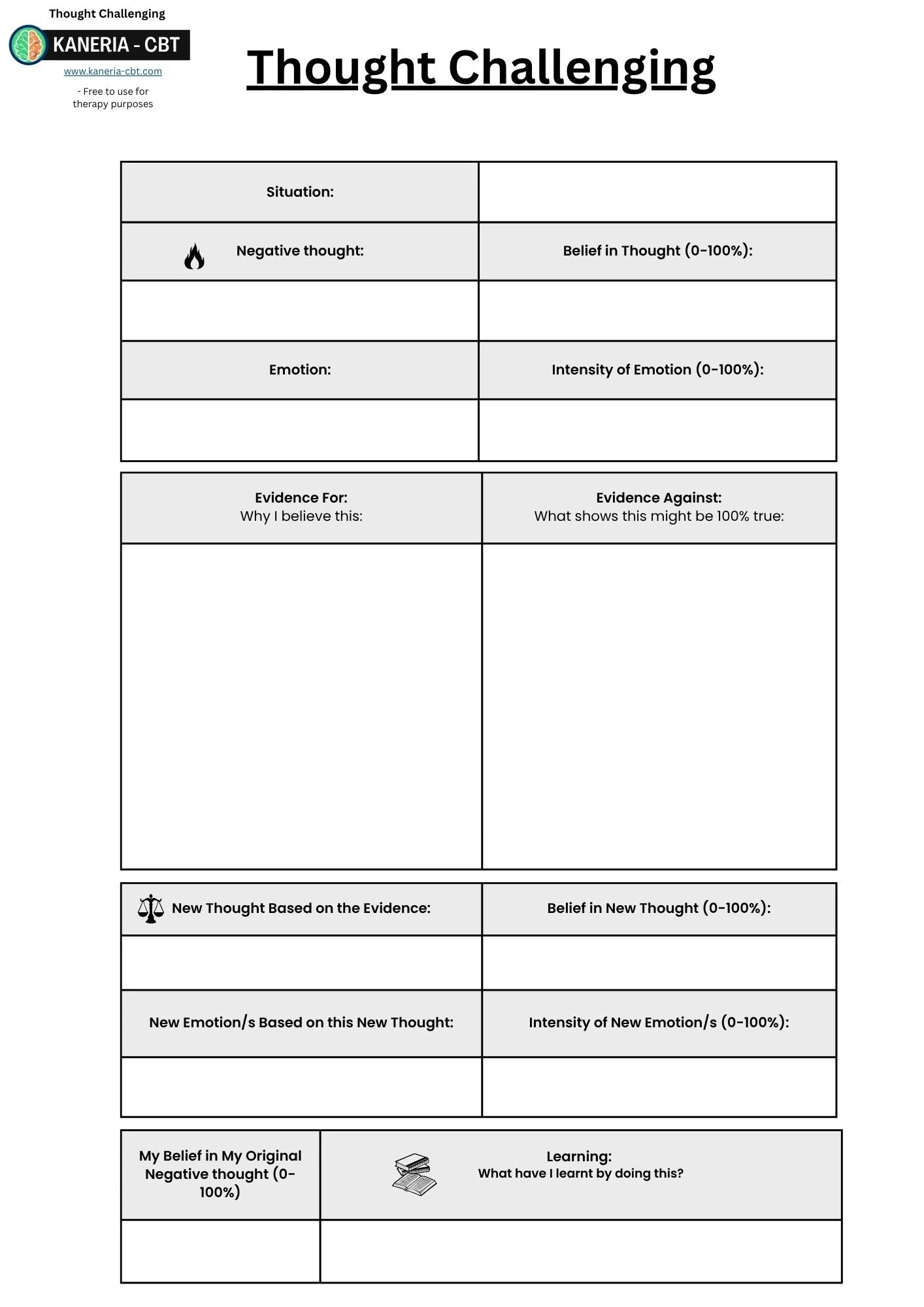
Cognitive Restructuring Worksheets:
These are free to use worksheets you can use with your patients.
Click the image to download the worksheet.
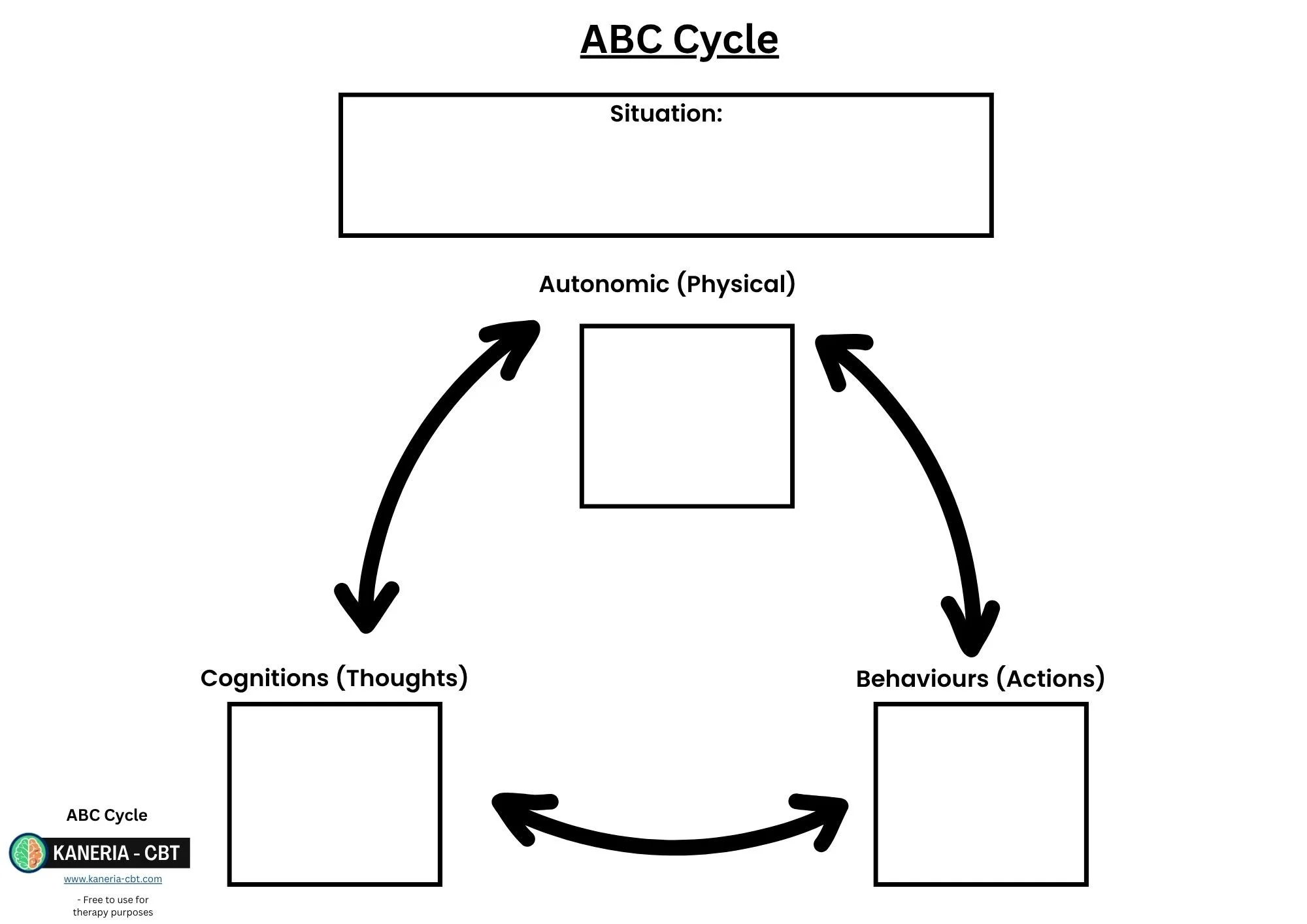
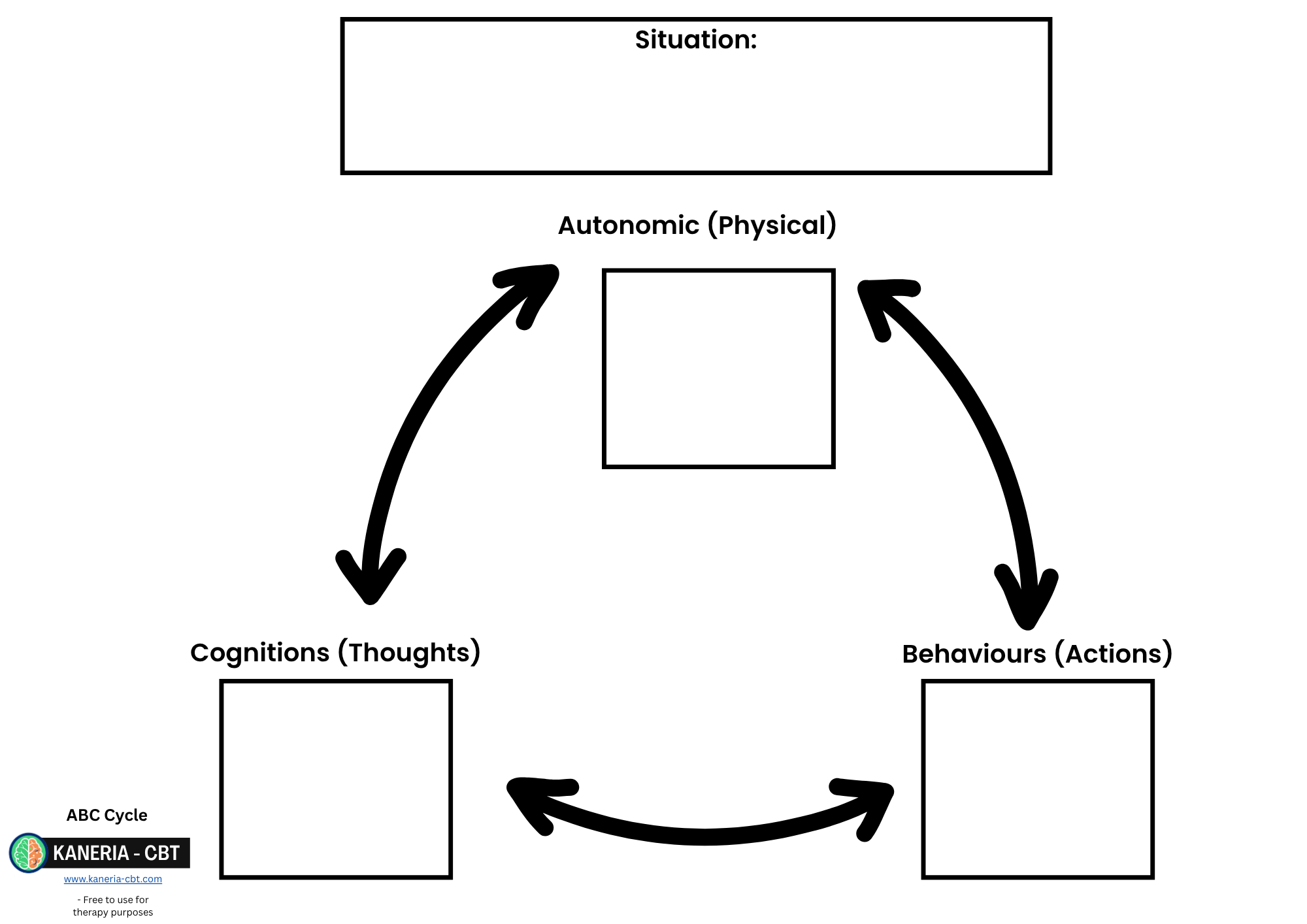
ABC Cycle:
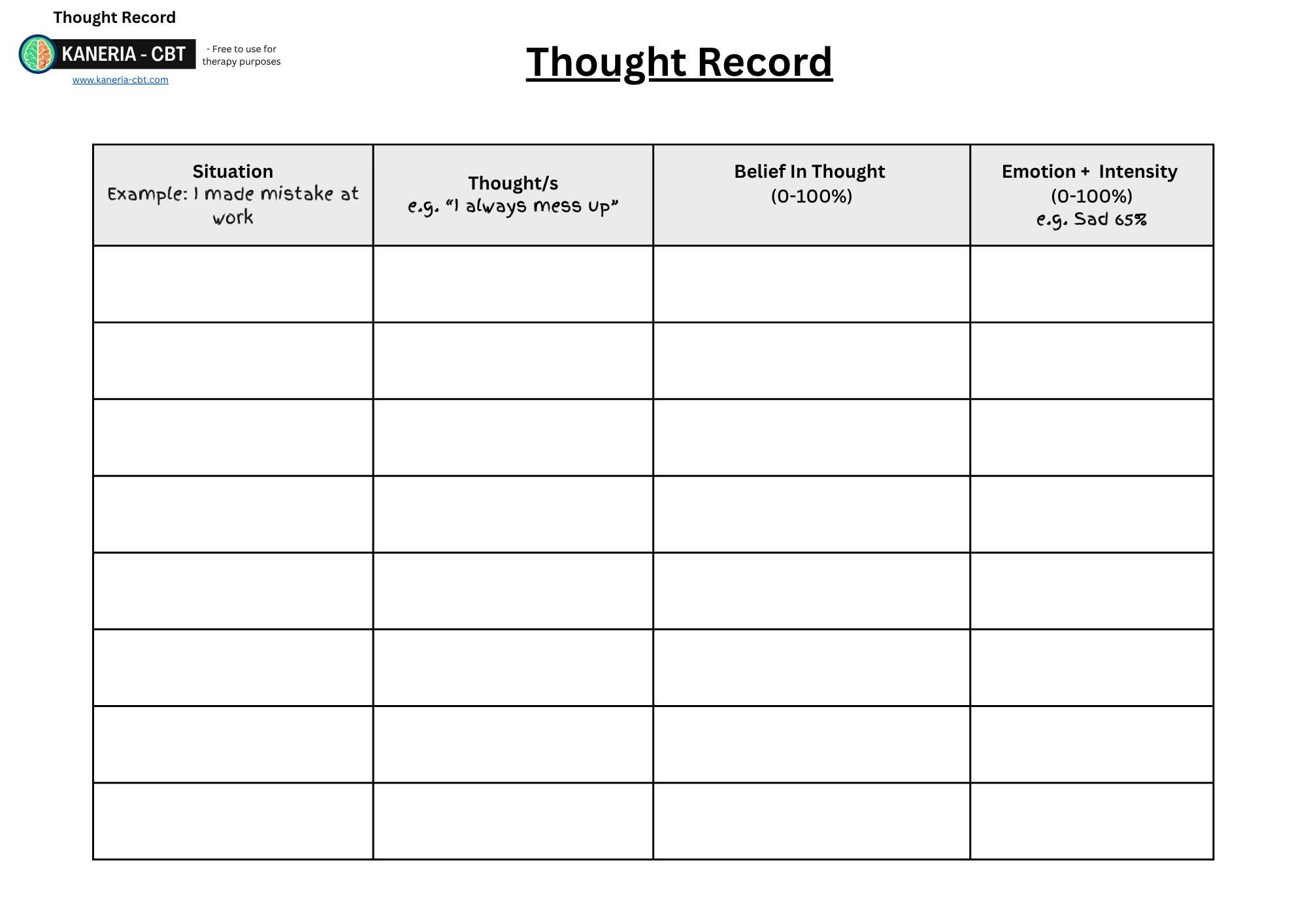
Thought Diary:
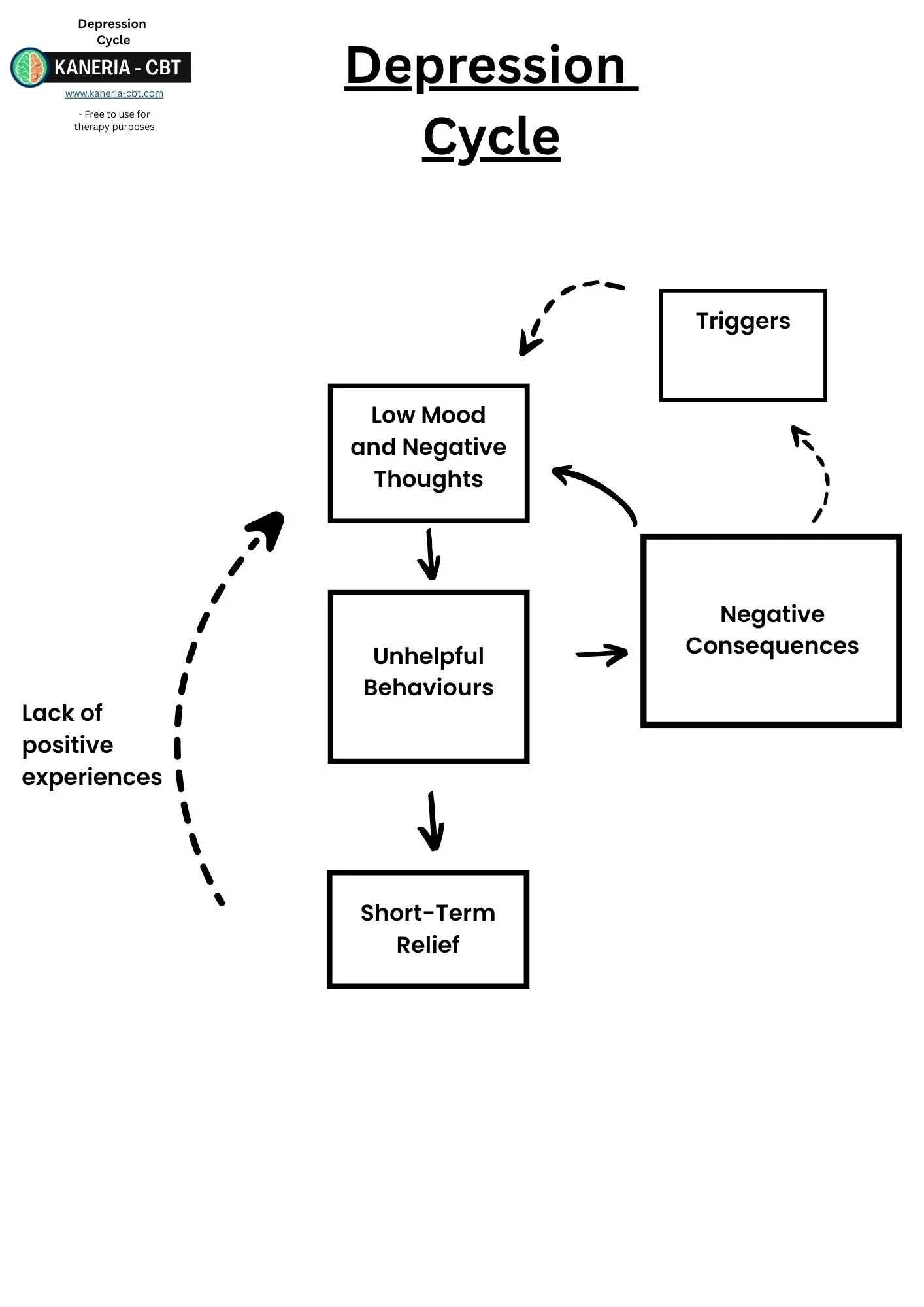
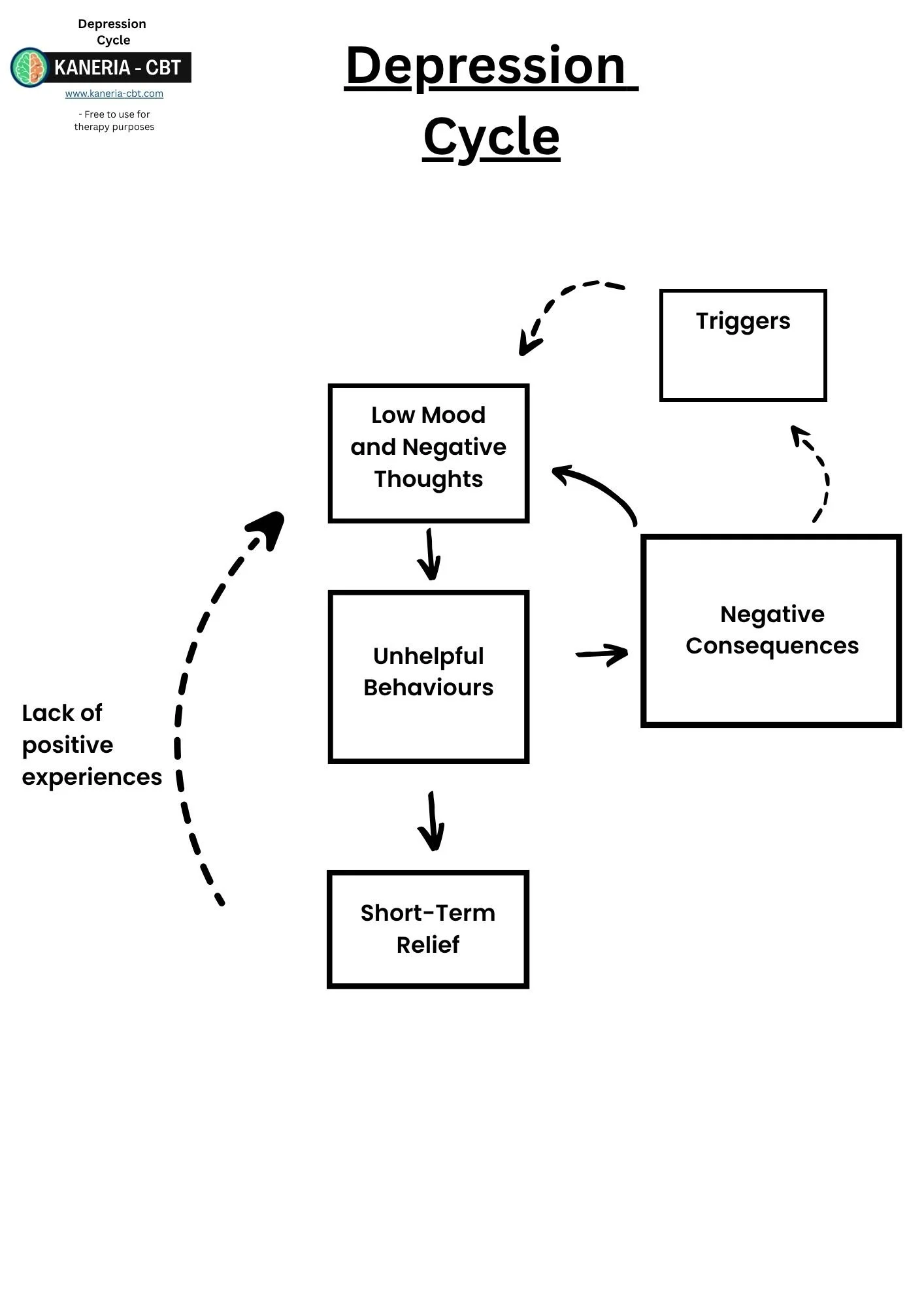
Depression Maintenance Cycle:
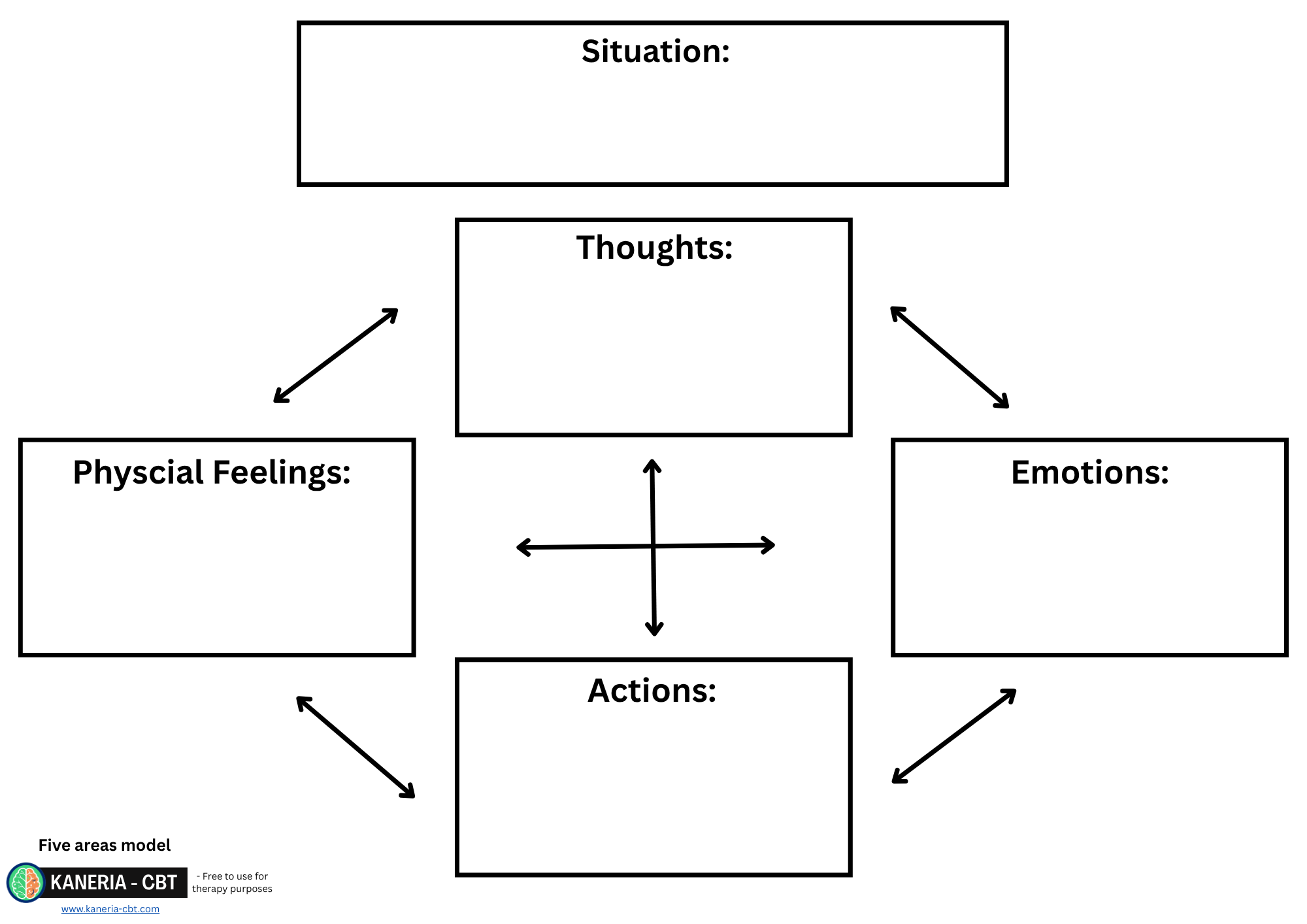
Five Areas Model:
Cognitive Restructuring Chart:
Cognitive Restructuring Guide:
The main rationale for what maintains depression when using cognitive restructuring is that:
Low mood causes us to feel less motivated. When this happens, we do a lot of unhelpful behaviours such as putting things off and doing less. This in turn creates less motivation and lower mood. This cycle reinforces itself and can be difficult for patients to naturally escape from.
This causes patients can often become self-critical about their lack of achievements due avoiding all their responsibilities or about other triggering situations in their life. Self-criticism can lead to an increase in cognitive distortions and negative thinking, which can maintain depression (Beck et al., 1979).
This means that one way to tackle depression is by looking at the cognitive distortions and negative thoughts caused by low mood. Once these thoughts are less distorted, patients are more likely to engage in more helpful behaviours and increase activity levels naturally. For this we used a strategy called Cognitive Restructuring (CR).
Cognitive Restructuring consist of 4 steps:
Step 1: Psychoeducation:
The first step consists of psychoeducation. Patients need to know about:
The ABC cycle or five areas model.
It is optional but helping the patient understand a maintenance cycle for depression is advised.
The difference between thoughts and opinions.
What “Negative Automatic Thoughts” (NATs) are.
What “Hot Thoughts” are.
Lets look at each of these:
ABC Cycle or five areas model.
The first step should also always be an ABC cycle or five areas model. Place more emphasis on the cognitions in this cycle.
ABC Cycle:
Five Areas Model:
Depression Maintenance Cycle:
It is optional but showing patients a maintenance cycle for depression can be helpful at helping them understand the rationale behind what maintains Depression and why treatment works.
There are many versions of this but they all show similar principles.
Triggers: Low mood can often be triggered by certain day-to-day situations.
Low Mood: These triggers cause your mood to dip causing our thoughts to become negative and often causing a lack of motivation.
Unhelpful Behaviours: When we are low, we often start to act differently. This can lead to unhelpful behaviours such as avoiding socialising, putting off tasks and doing less.
Short-Term Relief: When low, these tasks feel hard, therefore we get a sense of temporary relief from not having to do the activity. However, this is often quickly followed by guilt, feeling lower or self-criticism for not doing the task. This lowers mood and starts the cycle again. Furthermore, avoiding activities also stops us from having positive experiences which would help counteract the low mood.
Negative Consequences: Often these activities pile up and cause an impact on our life. We can put off responsibilities or stop engaging in meaningful activities. This can make our low mood worse, which starts the cycle again.
Thoughts vs opinions:
Following this, have a discussion with the patient if thoughts are accurate representations of the world. The answer is they are not. Using metaphors and thought experiments can be useful for this.
Example metaphor:
Ask the patient if they like or fear dogs. Whatever their answer is, ask them to imagine walking down the street with someone who is the opposite. A dog comes walking towards the two of you. One of you will be scared and have thoughts such as “the dog will bite me” and one will be thinking “aww what a cute dog”. Both people are seeing the same dog but having completely different experiences. This should demonstrate well that thoughts really can influence how we perceive the world.
This then can be linked to depression and that when we are feeling low, we have a tendency to see the worst or misinterpret the world in a negative way.
Help the patient understand that if they can change the way they are thinking. This can then change their emotions, and how they act in response.
Negative Automatic Thoughts (NATs):
One of the main psychoeducation points is what are NATs. As the name suggests these are Negative thoughts which occur automatically and almost instantly when a trigger occurs. An example of this could be the NAT “I am a terrible parent” after slightly raising their voice at their child.
Hot Thoughts:
This psychoeducation point can be saved for after the patient has completed their first thought record. A “hot thought” is a word used to describe the NAT that is most highly linked to the negative emotion the patient experiences within a situation. We often have many thoughts around a situation or topic. The “hot thought” allows us to focus and challenge the one causing the main impact without having to challenge every single thought the patient has.
Step 2: Identifying Unhelpful Thoughts:
The second step in CR is to get the patient to be able to recognise their own thoughts. NATs are automatic judgments and therefore are hard to recognise. This is because patients often feel the impact of their thoughts and instantly accept them as true.
To help with this the patient is recommended to keep a thought diary for the week in which they record any experiences of low mood. Various charts exist but most try to capture the:
Situation prior to the NAT: This helps the patient see their triggers and context for their thoughts.
Thoughts: The more they practise recording their thoughts, the easier they will find noticing their NATs. If a patient struggles with this, ask them what their views are on the situation or get them to focus on how they emotionally felt as they tell you more about the situation (this usually helps activate the NATs experienced).
Belief in thought (0-100%): The patient can rate how much from 0-100% they believed this NAT. This helps identify the hot thought and is also used later when challenging the thought. It also helps reinforce the idea that thoughts are not facts and are subject to change.
Emotion felt: The patient should aim to record their emotions. This can help the patient see a link between their thoughts and feelings.
Intensity of Emotion (0-100%): The intensity of the emotion can also be rated. This helps identify the hot thought.
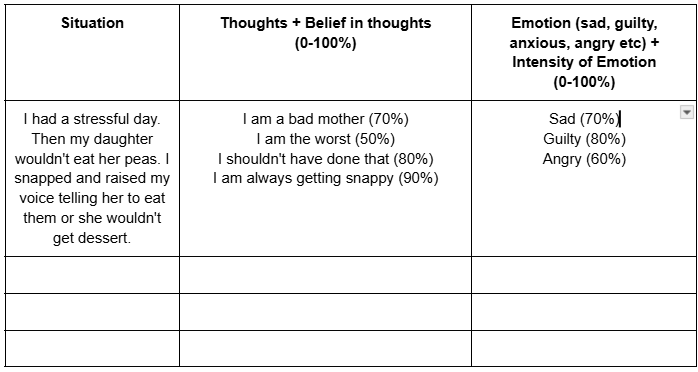
Here is an example thought record:
Thought records should be set for homework. It can also be useful to ask the patient to pause the session if they notice having a NAT in the session (or if they can recall if any occurred since the start of the session). This can help demonstrate how to fill out the chart together in session. Once the patient has filled out the chart, they need to select the “hot thought”. The best way to do this is look at what the highest emotion was and see which thought was most likely linked to it. In this patient's example the patient's strongest emotion was guilt at 80%. As you can see many of her NATs could be related to this. Ask the patient what they think is the most related thought. In this example case it was “I am a bad mother”. Check that the patient still believes their NAT before moving onto the next action. There is no point in challenging a thought that has been resolved or is no longer an issue.
Step 3: Gather evidence:
The next step is about evaluating the accuracy of the NAT. A crucial step before this, is to ensure the thought is phrased correctly to aid with challenging it. A NAT should be situation dependent. There is a big difference between “I am a bad mother (in general)” vs “I am a bad mother for shouting at my child situation specific)” when it comes to challenging this NAT. Trying to challenge a general idea is more difficult and may overlap with core beliefs, assumptions or rules, which step 2 CR is not designed for.
Once the NAT has been made situation dependent, the next stage is to look for evidence that supports the negative thought and then any evidence against it. Patients can really struggle with this section at first. Cognitive distortions can cause patients to not be able to recognise or accept evidence against their NAT. It is important to set up a few rules for what counts as evidence. Using inaccurate evidence can make the patient feel worse.
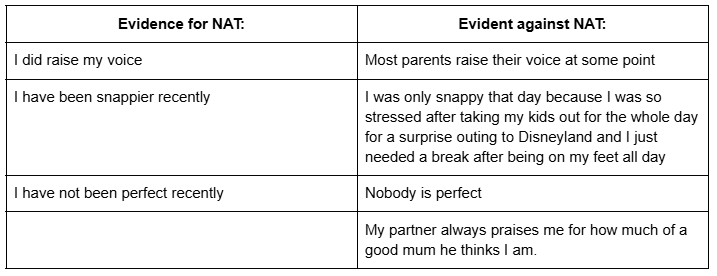
Example of evidence for and against the thought “I am a bad mother”:
Patients' evidence is likely to be distorted. One of the pieces of evidence used was “I did raise my voice” which is factually true. However, does it actually support the NAT of “being a bad mother” as much as the patient feels it does? Is everyone who raises their voice automatically a bad parent? You can get patients to tear down their evidence for their NAT by asking themselves a few simple questions such as:
Is your evidence for this based on facts or on how you feel?
Is this a realistic thought to have?
Could you be misinterpreting the evidence in any way?
Are you having this thought based on facts or is it a habit?
Are you seeing the big picture?
Are you looking at all the evidence or just what supports your negative view?
Are you exaggerating the evidence in any way?
Would your best friend agree with your interpretation?
Would this still be true if the same situation happened to someone else?
Did someone else make you believe this thought? Are they reliable?
Is the situation more complicated than you are viewing it?
Step 4: Creating New Balanced Thinking:
After looking at the evidence for and against, the patient can re-rate their belief in their original NAT and the intensity of emotion at this point. Once the patient has gone through all their evidence, they should be feeling slightly better and their belief rating should be lower than when it started.
If not, that is an indication that:
The patient has not gathered enough evidence against their NAT.
The patient has used bad evidence to support their NAT.
There is always the possibility their negative thoughts are accurate (rare). If so, maybe use problem solving.
The patient’s thought may be a core belief and may need a step up. This is one reason to keep a NAT situation dependent. Challenging a core belief of being a failure is hard, challenging a NAT of burning the toast is the reason for being a failure for example, is much easier.
This isn't to say a patient's belief in their NAT will go from 100% belief to 0%. You may only see a 10% drop. But that's still an improvement. Get the patient to realise that if they dropped it 10% today, what's to stop that from dropping another 10% next time, and the time after.
The next step is to come up with an alternative, more balanced thought to replace their NAT.
This step isn't about thinking positively, it's about a believable and accurate new view set in reality and based on the evidence used.
Based on the example we looked at:
“I am a bad mother” and be replaced with “I am not a bad mother for raising my voice. Occasionally, even good mothers shout at their children when really stressed”.
A new thought doesn't have to be positive such as “I am a good mother”, it can just counteract the original NAT.
Once an alternative thought has been created. Get the patient to rate how much they believe the new thought. This new view should make sense based on the evidence. If they don't believe it or it doesn't make sense, it's most likely just based on positive thinking rather than evidence.
Full CR Chart Example: All the charts previously shown are just sections from a bigger chart. A fully completed one should look similar to this:
Behavioural change:
Although not a direct part of CR, it is worth having a discussion on how, based on their new alternative thought, the patient can act next time a similar situation occurs, or how they can act now. This goes back to the ABC cycle. Changing cognitions should lead to a behavioural difference. Going back to our example for example, if the patient is not a bad mother for raising their voice occasionally, if they do so in the future, how can they respond differently (and not based on the old NAT of being a bad mother).
Behavioural change can also be a good way to test how true the new alternative is. Use this when the patient doesn't have much confidence in their new view. Test it out!
Written by David Kaneria
CBT Therapist & Previous Psychological Wellbeing Practitioner (PWP)
Author of Low-Intensity Cognitive Behaviour Therapy; A Psychological Wellbeing Practitioner (PWP) Handbook
Low-Intensity Textbook:
For more information on Cognitive Restructuring and much more, check out my PWP textbook on amazon.
Patient Depression Self Help Book:
If any patients could benefit from any further support after therapy to maintain their progress my self-help book contains all the step 2 depression strategies in one easy to understand book.